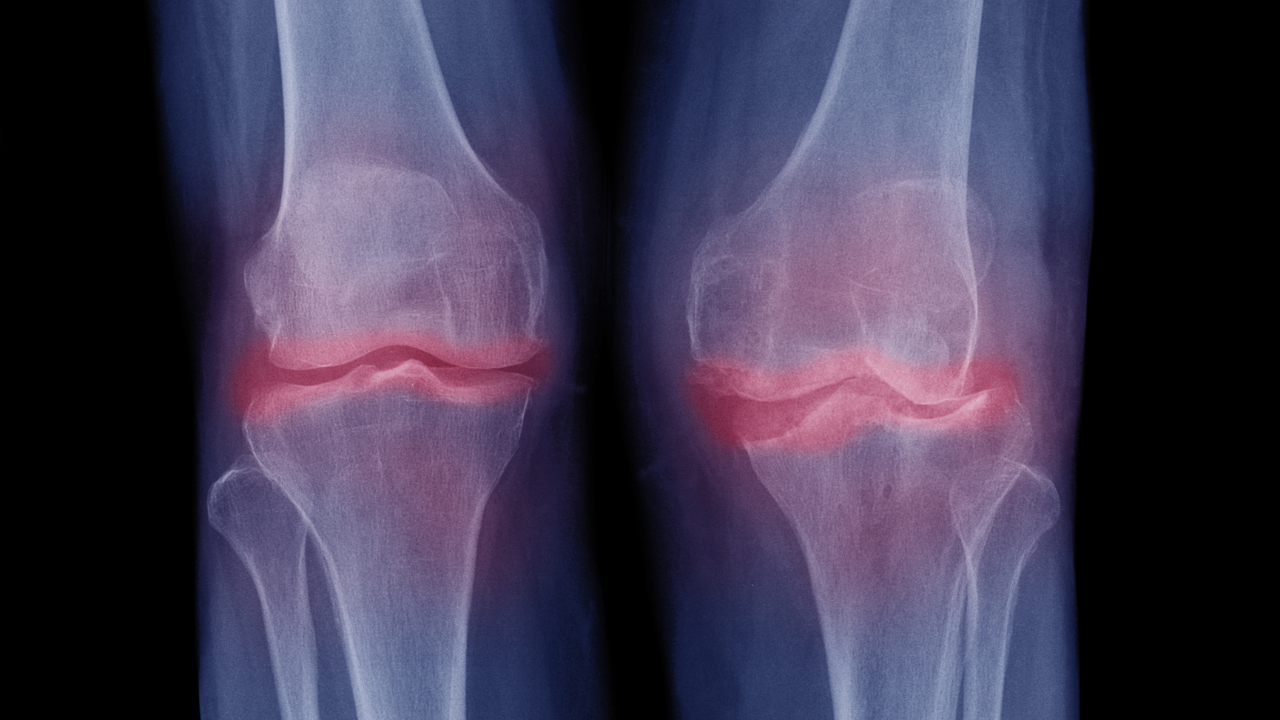
Knee Osteoarthritis
Knee osteoarthritis (OA) is a degenerative joint condition that commonly affects the knees. It’s the most prevalent type of arthritis and is marked by the gradual wearing down of cartilage that covers the ends of the bones in the knee. This degradation results in pain, inflammation, and reduced joint mobility.
Key Points About Knee Osteoarthritis
- Cartilage Breakdown: Cartilage serves as a cushion in the knee joint, facilitating smooth movement. In osteoarthritis, this cartilage gradually deteriorates due to factors such as aging, genetics, obesity, injuries, and joint overuse.
- Symptoms: Common symptoms include knee pain, stiffness, and swelling, especially after activities like walking, stair climbing, or standing up. Over time, the pain may become more persistent.
Do's
- Maintain a Healthy Weight: Managing your weight can reduce pressure on the knee joints, alleviating some of the symptoms. Focus on a balanced diet and regular physical activity.
- Stay Active: Engage in low-impact exercises like walking, swimming, or cycling to maintain joint flexibility and muscle strength. Consult a healthcare professional for tailored exercises.
- Regular Exercise: Strengthening muscles around the knee can improve joint support. Focus on exercises for the quadriceps, hamstrings, and calves.
- Use Assistive Devices: Knee braces, crutches, or canes can help reduce knee strain and improve movement.
- Practice Proper Posture: Maintaining good body alignment reduces unnecessary stress on your knees. Avoid standing or sitting for long periods in positions that cause discomfort.
Don’ts:
- Avoid Prolonged Inactivity: While rest is important during flare-ups, being inactive for too long can cause stiffness and muscle weakness. Strike a balance between movement and rest.
- Don’t Overexert Yourself: High-impact activities like running and jumping should be avoided as they can worsen knee pain.
- Limit High-Impact Exercises: Sports like basketball or tennis may increase stress on your knees. Opt for gentler activities that are easier on the joints.
- Don’t Ignore Pain: Listen to your body—if pain worsens, adjust your activity level accordingly.
- Avoid Deep Bending and Twisting Movements: Actions that require significant knee bending or twisting can strain the joint and exacerbate discomfort.
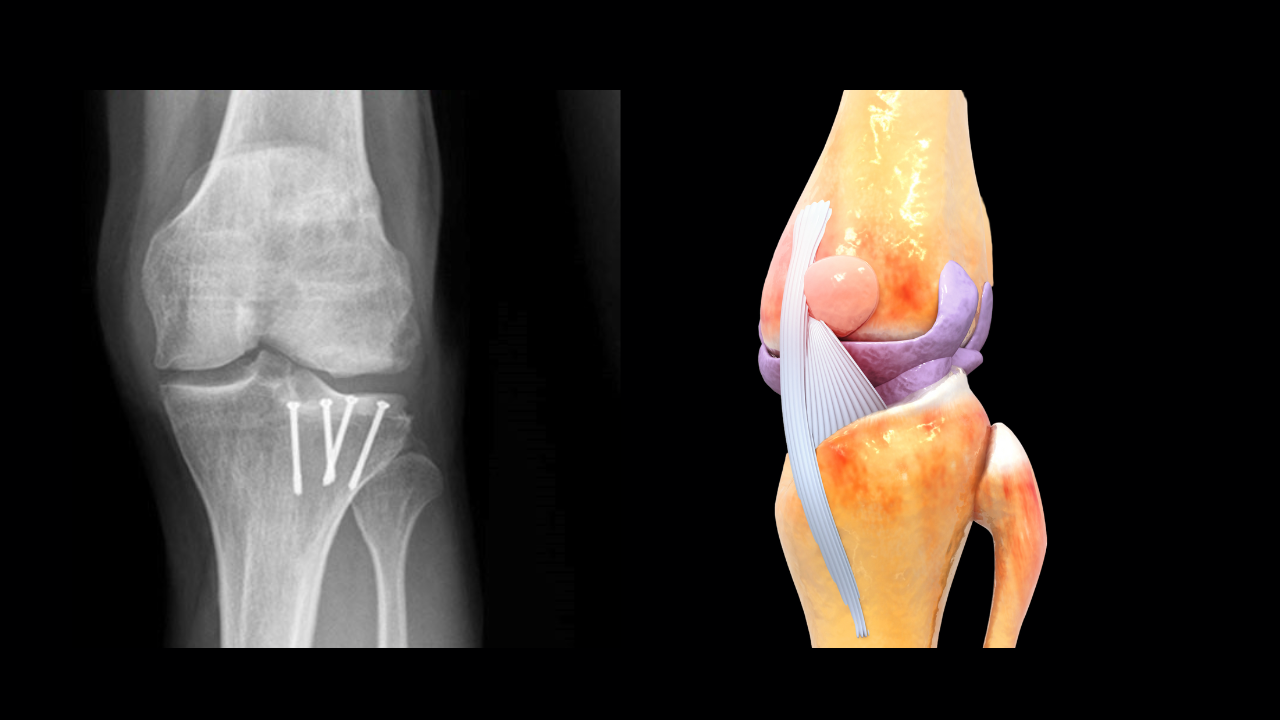
Joint Preservation Surgeries
Joint preservation surgeries are designed to maintain and prolong the function of a joint, especially in cases of early-stage joint damage or disease. These procedures aim to prevent or delay the need for total joint replacement by preserving the joint’s integrity. Joint preservation surgeries are typically considered for patients with conditions like osteoarthritis, avascular necrosis, or cartilage damage, where the joint has not yet suffered severe degeneration. These surgeries help alleviate pain, improve joint function, and slow down the progression of joint damage.
Common Joint Preservation Surgeries
Knee Arthroscopy:
High Tibial Osteotomy (HTO):
HTO involves cutting and realigning the upper tibia (shinbone) to redistribute weight away from the damaged part of the knee to a healthier area. This helps relieve pain and slows down the progression of conditions like medial compartment osteoarthritis, which affects the inner knee joint.
Distal Femoral Osteotomy (DFO):
DFO is similar to HTO but focuses on the femur (thighbone). It is performed to treat lateral compartment osteoarthritis, which affects the outer part of the knee joint. By adjusting the alignment of the femur, DFO redistributes weight and reduces stress on the damaged area, preserving the joint.
Do’s and Don’tsfor Joint Preservation Surgeries
Do's
- Follow Pre-Operative Instructions: Adhere to your surgeon’s pre-surgery guidelines, including fasting and medication restrictions.
- Prepare Your Home: Ensure your living space is recovery-friendly by creating clear pathways and having assistive devices like crutches ready if needed.
- Take Medications as Directed: Use prescribed pain relievers and antibiotics as instructed to manage discomfort and prevent infection.
- Keep Incisions Clean: Follow your surgeon’s care instructions to prevent infection and promote healing.
Don’ts:
- Don’t Overexert Yourself: Avoid putting excess pressure on the operated joint early in recovery. Gradually increase your activity level as guided by your physical therapist.
- Don’t Skip Physical Therapy: Consistently attending physical therapy is crucial for regaining strength and function in the joint.
- Don’t Ignore Signs of Infection: Contact your surgeon immediately if you notice fever, redness, swelling, or drainage from the incision.
- Avoid High-Impact Activities: Stay away from activities that may strain or damage the joint, such as running or jumping, during recovery.
Medical Management Overview
Physiotherapy:
Physiotherapy is a healthcare discipline focused on restoring and maintaining physical function, mobility, and strength. It employs exercises, manual therapy, and other techniques to enhance flexibility, muscle strength, and overall mobility. Physiotherapists assess individual conditions and create personalized treatment plans for issues like muscle strains, joint pain, post-operative recovery, sports injuries, arthritis, and neurological or respiratory disorders. By enhancing the body’s natural healing abilities, physiotherapy aims to improve functional capacity and overall quality of life.
Medication:
- Acetaminophen (Tylenol): Commonly prescribed for mild to moderate knee pain, acetaminophen provides pain relief without significant anti-inflammatory effects. It’s considered safe when taken at the recommended dose.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen, naproxen, and diclofenac are frequently used to alleviate pain and inflammation. While effective, long-term NSAID use should be monitored due to potential gastrointestinal or cardiovascular risks.
Weight Management:
Maintaining a healthy weight is essential for reducing stress on the joints, especially in cases of osteoarthritis. Excess weight can worsen symptoms and accelerate joint damage. Weight reduction, through exercise and physical therapy, can help improve flexibility, muscle strength, and joint function. Low-impact activities such as swimming and cycling are recommended.
Weight Reduction Medical Management:
Weight loss is critical for those struggling with obesity, particularly when lifestyle changes alone have been insufficient. Medical interventions include:
-
Prescription Medications: FDA-approved drugs can help with weight loss by reducing appetite or fat absorption. These are typically prescribed to individuals with a high BMI or weight-related health issues.
-
Behavioral Therapy: Counseling and behavioral therapy can help individuals address emotional eating and develop long-term healthy habits to support weight loss.
PRP Injections:
Platelet-Rich Plasma (PRP) therapy is a regenerative treatment that uses a patient’s own blood to promote tissue healing. After drawing and processing the blood, the platelet-rich plasma is injected into the affected area to encourage healing. PRP therapy is often used for conditions such as tendon injuries, ligament injuries, osteoarthritis, and chronic pain. While PRP is generally safe, its effectiveness varies, and insurance coverage for this treatment may be limited.
Frequently Asked Questions
How long does a knee replacement last?
A knee replacement can last 15 to 20 years or more, depending on factors such as the patient’s activity level, weight, and the type of implant used.
What is the recovery time for knee replacement surgery?
Most patients can resume normal activities within 6 to 12 weeks, but full recovery may take up to 6 months to a year.
Can I kneel after knee replacement surgery?
Kneeling may be uncomfortable after surgery, but it is generally safe. However, some patients may find it difficult to kneel due to stiffness or discomfort.
Is knee replacement surgery painful?
There will be some post-operative pain, but it can be managed with medications. Most patients report significant pain relief after recovery.
What is the difference between total and partial knee replacement?
Total knee replacement replaces the entire knee joint, while partial knee replacement only replaces one compartment of the knee. Partial replacement is less invasive and has a quicker recovery time.
What are the risks of knee replacement surgery?
Risks include infection, blood clots, implant loosening, and nerve damage. However, these risks are relatively low with modern surgical techniques.
How long will I need physical therapy after knee replacement?
Physical therapy typically lasts for 6 to 12 weeks, but some patients may require longer rehabilitation depending on their progress.
Can I drive after knee replacement surgery?
You can usually start driving 4 to 6 weeks after surgery, but this depends on which leg was operated on and how well you are recovering.
Will I need a walker or crutches after knee replacement?
Yes, most patients will need to use a walker or crutches for the first few weeks after surgery to help with mobility and balance.
Can I play sports after knee replacement surgery?
Low-impact activities like swimming, cycling, and golf are encouraged, but high-impact sports like running should be avoided to prevent damage to the new joint.
Discover New Heights in Healthcare with
Spire Hospital!

Address
Survey No 588, B4, 1st Floor, Ganesh Market, Jawaharlal Nehru Road, Aai Mata Mandir Chowk, Opp Market Yard Bus Depot, Bibevewadi, Pune : 411037
Phone
9175983868 / 8600159688
punehipandknee@gmail.com